By
Dr G Om Prakasham
Chairman, Lotus Wellness
Consultant Cardiac Surgeon
The liver is resilient and can regenerate itself by developing new cells. Each time a person drinks an alcoholic beverage, the liver filters the alcohol, liver cells die, and new cells develop. However, prolonged heavy drinking can gradually reduce the liver’s ability to regenerate itself, leading to permanent liver damage. While different substances can damage the liver, alcohol is one of the most common causes of liver damage.
How Alcohol Use Affects Your Liver
Drinking more alcohol than the liver can process damages the liver and can lead to liver disease. Alcohol contains ethanol, which has caloric value. However, the body cannot store alcohol for later use like it does fat and carbohydrates. Alcohol remains in body water until the body eliminates it, and it’s the liver’s job to oxidize alcohol for elimination.
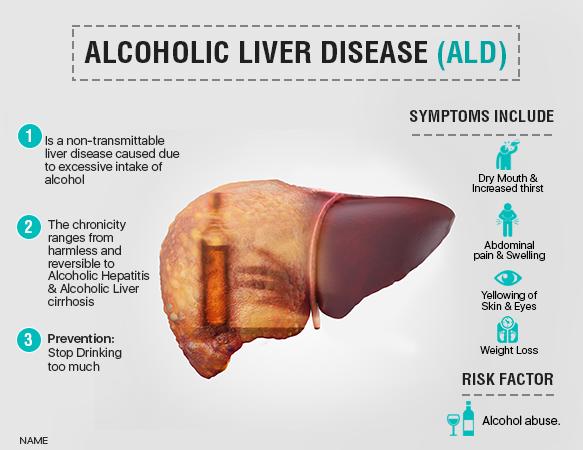
Alcoholic liver disease occurs when an individual engages in long-term heavy alcohol use, and there are three different types of liver disease. Alcohol-related liver disease can show up as any of the following conditions:
Fatty Liver Disease
The first stage of alcohol-related liver disease is fatty liver disease. Alcoholic fatty liver disease causes fat to build up in the liver. It occurs when an individual drinks a significant amount of alcohol, and it can develop even when someone drinks heavily for as little as a few days.
Fatty liver disease indicates a person is consuming harmful amounts of alcohol, but it is not always noticeable because it seldom causes symptoms. Symptoms can include mild discomfort in the abdomen’s upper right side caused by an enlarged liver.
Abstaining from alcohol use for two weeks can reverse fatty liver disease, and the liver should return to its normal state. However, continuing to drink excessively with fatty liver disease can lead to further stages of liver disease.
Alcoholic Hepatitis
Continuing to drink after developing fatty liver disease can further damage the liver and lead to alcoholic hepatitis. Alcoholic hepatitis differs from infectious hepatitis and causes the liver to become inflamed. When someone has alcoholic hepatitis, their liver becomes swollen and their liver cells die, often leaving scars on the liver. It can vary in severity, so one person may develop a mild case of it while another develops a severe one.
A mild case of alcoholic hepatitis may continue for years and gradually cause more liver damage if an individual continues drinking. Severe cases of alcoholic hepatitis occur suddenly and can be fatal. They typically occur after binge drinking, and the only way to prevent this condition from worsening and increase life expectancy is to abstain from drinking alcohol.
Alcoholic Liver Cirrhosis
Approximately 10%-15% of people who engage in long-term heavy or binge drinking eventually develop cirrhosis. Alcoholic liver cirrhosis typically develops after a decade or more of consuming alcohol. Scar tissue accumulates and replaces most of the liver’s cells, preventing them from regenerating.
This condition is irreversible and can progress to cause significant liver damage before a person experiences symptoms. Alcoholic liver cirrhosis can cause the following symptoms:
• Fatigue
• Itchiness
• Confusion
• Weakness
• Spider veins
• Muscle wasting
• Enlarged spleen
• Behavioral changes
• Pressure in the liver
• Decreased concentration
• Easy bruising and bleeding
• Bleeding veins in the esophagus
• Redness on the hands and palms
• Fluid retention in the legs and abdomen
Short-Term Effects of Alcohol Use
Short-term alcohol use can cause fatty liver disease, which is the first stage of liver damage. Fatty liver disease can go unnoticed because it rarely causes symptoms. In some cases, it can cause gastrointestinal symptoms, fatigue, weight loss and discomfort.
Alcohol use can also cause short-term effects such as:
• Headache
• Drowsiness
• Slurred speech
• Distortion of senses
• Altered mood or behavior
• Dehydration and muscle cramps
Long-Term Effects of Alcohol Use
Long-term alcohol use can cause serious health conditions such as:
• Stroke
• Cancer
• Heart disease
• Memory problems
• High blood pressure
• Weakened immune system
Long-term alcohol use can cause fatty liver disease to progress further, increasing damage and causing conditions such as alcoholic hepatitis and alcoholic liver cirrhosis.
Cirrhosis can eventually lead to liver cancer or fatal liver failure. Individuals with significant liver damage who meet specific criteria may find improvement with a liver transplant.
Early Signs of Liver Damage
Individuals in the early stages of liver damage seldom experience symptoms, so it often goes unnoticed. If symptoms do appear, they may include the following:
• Fatigue
• Nausea
• Vomiting
• Weight loss
• Low appetite
• Discomfort in the upper abdomen’s right side caused by liver swelling
Alcoholic fatty liver disease is the first stage of liver damage, and it can include symptoms such as discomfort in the liver, weight loss and fatigue. If alcohol consumption continues and further damage occurs, a person may experience additional symptoms such as a loss of appetite, nausea, vomiting and jaundice. Jaundice is a yellowing of the eyes and skin, so it can alter a person’s complexion and turn the whites of the eyes yellow.
Additional Risk Factors for Liver Disease
Heavy alcohol use is the main cause of alcohol-related liver disease, but certain factors can increase an individual’s risk of developing this disease. A person may be more at risk for alcohol-related liver disease because of the following:
• Gender: Women are more susceptible to developing alcoholic liver disease and experiencing its effects due to differences in body water content, metabolism and hormones. Estrogen levels can increase inflammation caused by liver disease, and a slower metabolism combined with a lower body water content can increase blood alcohol levels.
• Genetics: Alcohol use disorder can be hereditary, increasing the risk of alcohol-related liver disease for individuals with family members with alcohol addiction and liver disease.
• Age: Older individuals are also more susceptible to alcohol-related diseases because the body’s ability to metabolize alcohol decreases with age.
• Weight: Obesity can also increase the risk of alcohol-related liver disease.
• Infection: Chronic hepatitis C or hepatitis B can accelerate liver damage.
Complications of Liver Disease
Alcohol-related liver disease can cause the liver to lose its ability to function because of permanent scarring. It can also enlarge the veins in the esophagus, which is what causes bleeding in the esophagus. A person with liver damage may have increased blood pressure in the liver’s blood vessels and lose some brain function due to an accumulation of toxins in the blood. Liver damage can also cause malnutrition and shorten a person’s life span.
How Is Liver Disease Diagnosed?
Liver disease can be difficult to detect since it can develop without obvious symptoms, but early diagnosis is critical. Doctors will typically use imaging tests, tissue samples and blood tests to diagnose liver disease and determine the best treatment options because effective treatment depends on the extent of the damage.
If your doctor suspects you may have liver damage, they will begin by reviewing your health history and completing a physical exam. They may also recommend the following tests:
• Imaging tests: MRIs, CT scans and ultrasounds can detect liver disease and show the extent of the damage.
• Blood tests: Liver function tests are a series of blood tests that detect liver disease and check for certain liver problems.
• Biopsy: Doctors can remove a tissue sample from your liver to check for signs of damage and diagnose liver disease. During this procedure, a doctor will use a long needle to extract tissue from the liver and then send the sample to a lab for testing.
How Many Years of Drinking Can a Person Engage in Before Liver Damage Occurs?
There is no specific timeline for liver damage because it progresses gradually. Fat can begin to build up in the liver as soon as a person drinks a significant amount of alcohol, and continued drinking can lead to further damage.
Alcoholic liver disease can occur when a person consumes 30-50 grams of alcohol daily for over five years. However, different factors can affect when a person develops liver disease and when they start to experience symptoms. One person may develop liver disease within a few months of heavy drinking, while another develops it after a decade or two of heavy drinking.
Is Any Amount of Alcohol Safe?
The healthiest and safest amount of alcohol is no alcohol. The best way to protect your body from the short-term and long-term effects of alcohol is to abstain from it completely. Moderate drinking involves two or fewer drinks for men and one drink or less for women daily. While drinking in moderation is safer and healthier than binge drinking or long-term heavy drinking, it is still better to drink no alcohol at all.
How to Protect Your Liver
The liver can typically regenerate cells and recover from fatty liver disease as long as it has not progressed further. However, any scarring on the liver cannot be reversed. While some stages of liver damage cannot be reversed, protecting your liver can repair some damage, prevent the disease from worsening and increase your life span. You can prevent liver disease and protect your liver from further damage with the following strategies:
Reduce or Eliminate Alcohol Intake
The most effective way to protect your liver is to abstain from alcohol consumption. However, if you do drink alcohol, you can prevent liver damage by limiting your alcohol use to less than one or two drinks in a day and having regular alcohol-free days. If you have an alcoholic beverage, follow it with several non-alcoholic drinks to rehydrate your body.
Since it’s best to avoid alcohol, you can stop drinking by avoiding people who pressure you to drink and places that serve alcohol. Replace alcohol with other beverages such as water or non-alcoholic cocktails.
Live a Healthy Lifestyle
In addition to avoiding alcohol, some healthy lifestyle habits can help prevent liver disease and reduce its impact. You can benefit your liver by managing your weight with a balanced diet and regular exercise. It’s also important to avoid coffee, cigarettes and processed foods.
Recognize the Signs of Alcohol Addiction
Alcohol use disorder can make it difficult to abstain from drinking, so it’s important to recognize the signs of alcohol addiction. Recognizing the signs of alcohol use disorder can help you seek helpful resources to stop drinking. You may have an alcohol use disorder if you experience the following signs and symptoms:
• Frequent alcohol use
• Intense alcohol cravings
• Struggling to stop drinking
• Consuming more alcohol than intended
• Allowing alcohol to keep you from enjoying hobbies
• Continuing to drink when it interferes with relationships
• Spending significant time drinking or purchasing alcohol
• Engaging in dangerous behavior such as drinking while driving
• Allowing alcohol to interfere with work, school or home obligations
• Developing a tolerance and needing more alcohol to feel the same effects
Get Help
If you struggle to avoid alcohol or limit your alcohol consumption, help is available. With treatment, you can stop drinking and gain freedom from addiction. Avoiding alcohol can help you prevent liver disease or treat existing liver damage to live a healthier life and increase your life span. Seeking treatment for alcohol use disorder is the first step toward getting your life and health back.
ABOUT LOTUS WELLNESS
Lotus is the most featured Wellness and Rehabilitation Center in Coimbatore , India , offering the best programs for Detox , Deaddiction and Absolute Wellness.
WE ARE HERE FOR YOU
We at Lotus would be glad to help you or loved one overcome his or her Addiction and stand up for recovery
LOTUS WELLNESS AND REHABILITATION CENTER
Pollachi, Coimbatore , Tamilnadu , India
Call confidentially 24/7 (+91 7339062555)
Reach us at info@lotuswellness.life
To know more about us visit our website
www.lotuswellness.life